Ethical Health Care: Real Principles You Can Use
Ethical health care isn’t an abstract idea. It’s how people are treated when they walk into a clinic, how decisions are made during a crisis, and how systems share resources. During the COVID years, ethics mattered more than ever—who got a ventilator, who got tested, who got paid leave. Those choices reveal what a system values.
Ethics starts with fairness. That means equal access to care regardless of race, income, or where you live. It also means clear rules for tough choices, like ICU beds or vaccine distribution. When rules are clear and public, trust grows. When they’re hidden or biased, people lose faith fast.
Core principles everyone should know
First, respect patient autonomy. Ask people what they want, explain options, and get clear consent. Second, do no harm—clinicians should avoid treatments that hurt more than they help. Third, justice: distribute care and resources so no group is left behind. Fourth, transparency: explain how decisions are made and why. Finally, cultural competence: care must fit the person’s background and needs.
These sound simple, but practice matters. Cultural competence can mean offering interpreters, training staff on bias, or adjusting communication for different communities. Addressing racial bias in medicine isn’t just a moral step— it changes outcomes. Patients who feel heard follow treatment plans better and return for preventive care.
Practical steps for providers and communities
Providers can start by reviewing policies through an equity lens. Ask: who benefits and who might lose out? Train staff on implicit bias and on clear communication. Use checklists for high-stakes decisions so choices aren’t made on the fly. Make data public when possible—who is getting care, who isn’t, and why.
Communities should demand clear information. Ask local clinics about their triage rules and vaccine plans. Push for mobile clinics or community outreach where transport or cost barriers exist. Support free or low-cost testing and vaccination drives; small steps reach people who might otherwise fall through the cracks.
On financing, ethics shows up in the debate over free vs paid care. Free care can improve access but needs sustainable funding. Paid models can offer quality but leave vulnerable groups exposed. A mixed approach—public basics with options for extra private services—can balance fairness and quality if it’s governed transparently.
Finally, patients have power too. Speak up about concerns, ask for explanations, and bring a friend or advocate if needed. Know your rights and raise issues when care feels biased or dismissive. Change often starts with one voice insisting on fair treatment.
Ethical health care is practical work, not a slogan. Clear rules, honest communication, cultural awareness, and fair funding make health systems work better for everyone. Start small, keep asking questions, and demand systems that treat people with dignity.
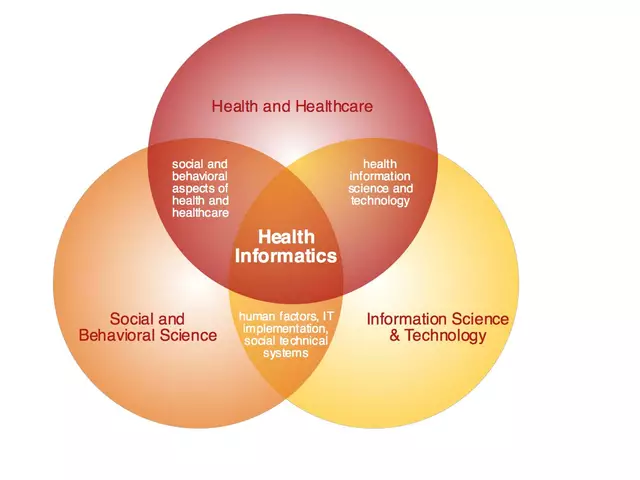
What is ethical based health care/medicine?
Posted by Finnegan Beckett On 8 May, 2023 Comments (0)

As a blogger, I've recently come across the concept of ethical-based health care/medicine, and I find it quite intriguing. Essentially, it refers to the practice of providing medical care based on moral principles and values, such as respect for autonomy, non-maleficence, beneficence, and justice. This approach emphasizes the importance of respecting patients' rights and ensuring their well-being while considering the potential consequences of medical decisions. By adhering to these ethical guidelines, health care providers aim to offer the best possible care while maintaining a strong moral compass. I believe that ethical-based health care can greatly enhance the overall patient experience and ultimately lead to better health outcomes.