Cultural competence in healthcare: improve patient care
Cultural competence in healthcare means understanding and respecting differences that affect a person's health, choices, and how they use services. In India and other diverse communities, culture shapes language, family roles, health beliefs, and trust in doctors. When care ignores those factors, patients miss out and outcomes suffer.
Start listening. Ask open questions about beliefs, family decision makers, and language needs. Small changes, using plain language, confirming understanding, or offering an interpreter, cut wasted visits and medication mistakes. Plain, direct questions like "Who helps you make health choices?" or "How do you prefer we explain this?" work better than guessing.
Learn common cultural practices that affect care in your area. That doesn't mean memorizing every custom, but knowing local patterns helps. For example, dietary habits, fasting practices, community roles, and attitudes toward mental health can change how you schedule tests, advise on medicines, or suggest follow-up. If you work in COVID care, understand vaccine hesitancy roots in religion, past experience, or misinformation, and address them respectfully.
Build trust with gestures that matter. Greet people in a way they expect, respect same-gender exam preferences, and show patience for family involvement. Trust is practical: it increases adherence to treatment, keeps people coming back, and reduces emergency visits. A quick note in the chart about a patient's preferred name, language, or decision maker saves time and prevents awkward moments.
Train the whole team, not just doctors. Nurses, reception staff, and community health workers meet patients first. Role-play simple scenarios: responding to a patient worried about a traditional remedy, or asking a family to step out when a private exam is needed. Practice short phrases in common languages and how to request an interpreter.
Use tools and tech smartly. Translation apps help in a pinch, but trained interpreters are best for complex conversations. Visual aids, videos, and easy-to-read handouts increase understanding. Track cultural needs in your records so follow-ups respect them; don't repeat the same barriers next visit.
Patient safety ties to cultural competence. Asking about herbal medicines, religious fasting, or home remedies prevents harmful drug interactions. Screening tools should be adapted so they don't misread symptoms that present differently across cultures. If a patient prefers a family elder to speak for them, document it and verify consent practices.
Patients can help too. Bring a list of medicines, tell providers about customs that matter, and ask for an interpreter when needed. If you're unsure, say so; most providers will welcome the chance to learn.
Cultural competence is not a one-time goal. It's a set of habits: listen, ask, adapt, and record. Those habits make care safer, cheaper, and more respectful. Start small, train consistently, and measure changes like fewer missed appointments or higher patient satisfaction. That's how care actually improves.
If you work in public health or run a clinic, set simple goals: collect language data, schedule cultural training, and ask patients for feedback after visits; small moves build change over time and help track results better.
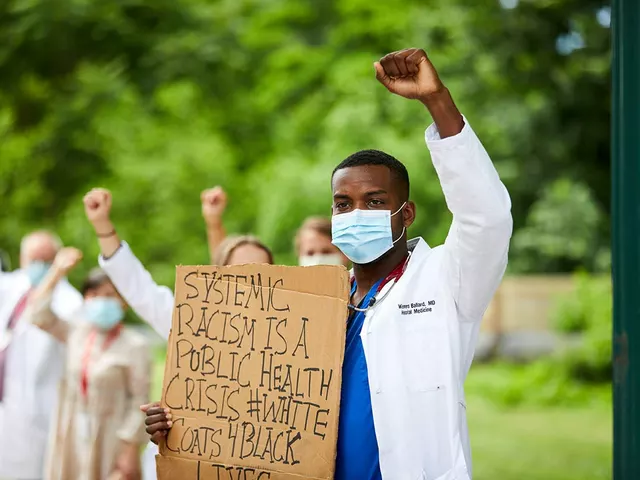
Addressing Racial Bias in Medicine - Improving cultural competence in health education
Posted by Finnegan Beckett On 27 Jul, 2023 Comments (0)

Well folks, buckle up because we're diving headfirst into the complex world of racial bias in medicine - it's a wild ride! Addressing this often unseen elephant in the room can have transformative impacts on health education and, ultimately, patient care - it's like turning a health kaleidoscope and seeing a whole new perspective! Improving cultural competence is like adding a secret ingredient to the health education recipe, it's about understanding, respecting, and valifying diverse patient backgrounds. And boy, it's not only about fixing the bias, it's about busting out a new dance move called 'empathy' and shaking up the traditional healthcare rhythm. So, let's put on our thinking caps, lace up our boots and march towards a health education system free of racial bias - it's going to be a heck of a journey, but together, we can make it happen!